In my message from March 10, 2020, I reported on the neuroinvasive potential of SARS-CoV-1 and other coronaviruses, a topic that has been well studied since 2003 (Dutch version: see "Verspreiding en complicaties van coronavirussen", 7 maart 2020). The neuroinvasive potential of SARS-CoV-2 has been underestimated since the beginning of this pandemic. Reasonably, it has been questioned whether neurological manifestations are a result of neuroinvasion by the pathogen SARS-CoV-2, or a result of thromboinflammatory events induced by SARS-CoV-2.
Due to a lack of autopsy specimens, viral replication of SARS-CoV-2 in the CNS cannot be confirmed. That is no reason to not raise awareness on the CNS and PNS invasive potential of SARS-CoV-2. Aside from direct neuroinvasion of the CNS, neurological manifestations evoked by inflammation and coagulation disorders (thrombosis and embolism) should be monitored closely. In this review, I will elaborate on the neuroinvasive potential of coronaviruses, neurological manifestations and mechanisms behind CoV-CNS infection. What is the point in drawing a distinction between neurological manifestations that start with direct invasion of the CNS or CNS manifestations mediated by inflammation in the periphery (outside of the CNS)? It is of relevance in respect of therapeutic options and timing of medical intervention.
1. On the neuroinvasive potential of coronaviruses (2016-2020);
2. Neurological manifestations concerning viral infection;
2.1 Manifestations of the nervous system in SARS-CoV-2 patients;
2.1.1 Encephalopathy;
2.1.2 MRI-findings in absence of specific CSF findings: unspecific encephalitis;
2.1.3 Unusual microbleeds;
2.1.4 Systemic hyperinflammatory CNS dysfunction;
2.1.5 Leukoencephalopathy and microhemorrhages (punctate bleedings);
2.1.6 Acute Necrotizing Encephalopathy (ANE);
2.1.7 ANE successfully treated with steroids;
2.1.8 Meningitis/encephalitis associated with SARS-CoV-2 infection of the Nervous System;
2.1.9 ADEM (Acute Disseminated encephalomyelitis): 2 cases of improvement after Methylprednisolone or Dexamethasone;
2.2 Markers for severe infection;
3 Mechanisms
3.1 Penetration or avoidance of the Blood Brain Barrier and Blood Nerve Barrier;
3.2 Dissemination through neural olfactory (smell and taste) connections
1. On the neuroinvasive potential of coronaviruses (2016-2020)
Like respiratory viruses in general, SARS-CoVs can cause damage to the central nervous system. Coronaviruses can induce encephalitis, as accumulation of interleukin-6 increases the permeability of the blood-brain barrier. The rapid replication of SARS-CoV-2 is a risk factor for initiating overreaction of the human immune system; viral meningitis can occur as a consequence (Human Coronaviruses and other respiratory viruses: Underestimated opportunistic pathogens of the Central Nervous System?, Viruses 2020, 12 (1), 14, published December 20, 2019). In a young patient group with CoV, a slight accumulation of IL-6, IL-8 and MCP-1 in the brain fluid was observed. MCP-1 is involved in initiating inflammatory responses in the brain (Coronavirus infections in the Central Nervous System and respiratory tract show distinct features in hospitalized children, Intervirology 2016, vol. 59, no. 3, published in February 2017).
In this 2016 study, a distinction was drawn between Coronavirus-CNS infection (CoV-CNS) and CoV-respiratory tract infection. The serum level of Granulocyte macrophage colony-stimulating factor (GM-CSF) was higher in CoV-CNS infected patients. GM-CSF has proinflammatory properties and plays a role in autoimmune encephalopathy. Levels of IL-6, IL-8, MCP-1 and GM-CSF were higher in cerebrospinal fluid samples of the CoV-CNS patient group. Lymphocyte and eosinophil counts were reduced in the CoV-CNS group, whereas CoV-respitatory tract patients had a significantly lower neutrophil cell count. The monocyte count in CoV-CNS was elevated. Notably, the serum level of Granulocyte colony-stimulating factor (G-CSF) was significantly elevated in CoV-CNS and CoV-respiratory infection alike.
Autopsies performed during the SARS-CoV-1 epidemic revealed viral RNA in the cytoplasm of hypothalamic and cerebral cortical neurons, as well as brain edema and focal neuronal degeneration and neuronal necrosis, extensive glial cell hyperplasia and cellular infiltrates. No demyelination was reported. Interferon-gamma was expressed in glia, infiltration of CD68+ macrophages and CD3+ T-cells was observed in brain neurons and glia (The neurology of COVID-19 revisited: A proposal from the Environmental Neurology Specialty Group of the World Federation of Neurology to implement international neurological registries, Journal of Neurological Sciences 414 (2020) 116884).
In ACE2 transgenic mice models, respiratory failure has been attributed to medullary infection with SARS-CoV. While little cellular infiltration was observed, the entry for viral infection of the brain was the olfactory nerve. One report on COVID-19 encephalitis reveals hemorrhagic rim enhancing lesions within the thalami, medial temporal lobes and subinsula. The potential for viral-induced vasculitis via brain endothelial ACE2-receptors increases the risk of cerebrovascular disease (COVID-19 and the nervous system, Journal of Neurovirology, 2020 May 23).

2. Neurological manifestations concerning viral infection
There are at least three categories of neurological manifestations associated with viral infection. Encephalopathy, inflammatory encephalitis, hemorrhagic and ischemic stroke are complications of systemic diseases, such as Multi Organ Failure, inflammation and coagulation. Direct viral invasion of the CNS results in encephalitis, meningitis and endotheliitis associated with cell necrosis and dysfunction. Acute Disseminated Encephalomyelitis (ADEM), Acute Necrotizing Encephalopathy (ANE), Guillain-Barré Syndrome and Kawasaki-like manifestations are immune-mediated post-infectious manifestations.
2.1 Manifestations of the nervous system in SARS-CoV-2 patients
In a case study involving 214 patients with SARS-CoV-2, neurologic symptoms were seen in 36,4% of patients. Mean age of patients was 52 years. Of all reported patients with nervous system manifestations, 24,8% had CNS manifestations, 8,9% had Peripheral Nervous System manifestations and 10,7% had skeletal muscle injury. Typical Peripheral Nervous System symptoms are anosmia and ageusia (loss of smell and taste). Notably, 58,9% of patients with CNS manifestations had nonsevere infection. Neurologic manifestations occurred within 1-2 days of the infection. 2 patients were admitted to the hospital with SARS-CoV-2-induced hemiparese, of whom none had fever, cough or diarrhea. Of CNS manifestions, headache, impaired consciousness, acute cerebrovascular disease, coma, delirium, ischemic stroke and cerebral hemorrhage were reported.
2.1.1 Encephalopathy
In a study concerning 58 patients, 69% had agitation, 67% had diffusive corticospinal tract signs and 33% had dysexecutive syndrome consisting of attention difficulties, disorientation and poorly organized response movements. In 8 patients, enhancement in leptomeningeal spaces was noted; in 11 patients, bilateral frontotemporal hypoperfusion was noted. 1 of 8 patients had diffuse bifrontal slowing consistent with encephalopathy; in 2 patients, oligoclonal bands were present, protein and IgG levels were elevated in 1 patient. RT-PCR arrays of the Cerebrospinal Fluid (CSF) were negative for SARS-CoV-2. Pleocytosis was not observed in any of the cases. This study concludes that ARDS due to SARS-CoV-2 infection was associated with encephalopathy, agitation, confusion and corticospinal tract signs. However, no conclusions can be drawn with regards to inflammation-mediated encephalopathy, as no cytokine arrays were performed (Neurologic Features in Severe SARS-CoV-2 Infection, NEJM, 4 June 2020).
2.1.2 MRI findings in absence of specific CSF findings: unspecific encephalitis
A study investigating 50 patients reports that the most common finding was cortical signal abnormalities on Fluid-Attenuated Inversion Recovery (FLAIR). In 3 patients, accompanying subcortical and deep white matter signal abnormalities were present; abnormalities in the frontal lobe were present in 4 patients; parietal lobe in 3; occipital lobe in 4; temporal lobe in 1; insular cortex in 3 and cingulate gyrus in 3 patients. CSF array of 5 patients revealed total elevated protein in 4 patients. Cell count, albumin, glucose levels and IgG Index were within normal range, no oligoclonal bands were observed. Acute intracranial findings in the absence of cortical signal abnormality included 1 patient with acute transverse sinus thrombosis and 1 patient with acute infarction in the right middle cerebral artery territory. Of 2 cases without intracranial findings, elevated protein was found in the CSF. The main differential diagnosis of these findings is infectious or autoimmune encephalitis, seizure, hypoxia and hypoglycemia. The cases of bilateral frontal involvement may have hypoexia as underlying pathogenesis, as ARDS and frontotemporal perfusion are associated factors. Cortical microhemorrhage and breakdown of the Blood-Brain Barrier accompanied by hypoxia are thought to result in the observed imaging pattern. Overall, no conclusions can be drawn with regards to viral or immunity-mediated encephalitis (Brain MRI Findings in Patients in the ICU with COVID-19 Infection, RSNA Radiology, 8 May 2020).
2.1.3 Unusual microbleeds
MR images of 9 patients with a common pattern of unusual findings are reported. All patients suffered from severe hypoxemia secondary to ARDS, with a delayed recovery of consciousness after sedation. None of the patients were reported to have Diffuse Intravascular Coagulation (DIC); all patients presented a hyperfibrinemic state as well as septic or inflammatory coagulation. Microbleeds were observed in unusual distribution with a specific tendency for the corpus callosum. Other locations of microbleeds were the posterior or anterior limbs of internal capsule and middle cerebellar peduncles. In the majority of the patients, subcortical regions were affected. These findings are assessed to be distinct from hypertension and amyloid angiopathy. The involvement of the corpus callosum is inconsistent with hypertension and amyloid angiopathy; short episodes of hypertension occurred in 2 of 9 patients, who were successfully treated with antihypertensives. It is hypothesized that direct damage to the endothelium and vessels could be explanatory, as direct interaction between SARS-CoV-2 and the ACE2-receptor could lead to damage of the Blood-Brain Barrier and bleeding within the brain tissue. Some of the lesions observed on MR imaging were reported to have a lineal shape resembling a vessel, which could represent microthrombi within vessels, consistent with hypercoagulation disorders and microthrombi in pulmonary vessels of other patients. Lastly, diffuse axonal injury or lipid embolism are explored as possible explanations (Unusual Microbleeds in Brain MRI of COVID-19 Patients, Journal of Neuroimaging, 8 July 2020).
2.1.4 Systemic hyperinflammatory CNS dysfunction
1 patient without comorbidities presented with left-sided paresthesias, a 1-day history of headache and ipsilateral paresis progressing within 12 hours to confusion and agitation. CSF showed lymphotic pleocytosis and increased proteins. PCR of SARS-CoV-2 in CSF returned negative, but positive in the nasopharyngeal swab. A second patient presented with agitation, difficulties naming objects, temporospatial disorientation and confusion. CSF showed lymphotic pleocytosis and increased proteins. In both patients, IL-6 was elevated, in one patient IL-1β was significantly elevated. In addition, CSF showed elevated levels of ACE in both patients. It is hypothesized that these cases of encephalitis are triggered by a cytokine storm. Treatments targeting IL-6 (tocilizumab) and IL-1 (anakinra) could be of benefit to treat CNS dysfunction (Increased CSF levels of IL-1β, IL-6 and ACE in SARS-CoV-2-associated encephalitis, Neuroimmunology & Neuroinflammation, 1 July 2020).
2.1.5 Leukoencephalopathy and microhemorrhages
11 patients were indicated for brain MRI for persistently depressed mental status. Brainstem reflexes were preserved, response in extremities was diminished. None of the patients had overt Disseminated Intravascular Coagulation. CSF was available in only 1 patient and was negative for infectious or inflammatory meningitis and encephalitis and was negative for SARS-CoV-2 on RT-PCR array. Of 11 patients, 4 patients presented with diffuse leukoencephalopathy, 1 with microhemorrhages and 6 with both microhemorrhages and leukoencephalopathy. Patients with leukoencephalopathy had symmetric hyperintensities involving bilateral deep and subcortical white matter. Abnormalities were observed to extend from the precentral gyrus down to the centrum semiovale and corona radiata. At the temporal and occipital horns, the posterior cerebral white matter was involved in all patients, notably more than the anterior white matter. The deep grey nuclei were spared from leukoencephalopathy. Apart from the pre-central gyrus and occipital lobes, the juxtacortical white matter was spared from leukoencephalopathy. These findings are reported to be consistent with Delayed Posthypopoxic Leukoencephalopathy (DPHL), occurring 10-14 days after hypoxic insult and similar to a pattern in carbon monoxide poisoning victims. The sparing of juxtacortical white matter and deep grey nuclei rules out acute hypoxic ischemia. DPHL is likely related to oligodendroglial cell death and subsequent demyelination. Observed mild restricted diffusion in this study can be related to acute demyelination. Possible etiologies for the observed leukoencephalopathy are sepsis-associated, post-infectious demyelating or hemorrhagic encephalitis and posterior reversible encephalopathy syndrome.
Punctate microhemorrhages were seen in the juxtacortical white matter and corpus callosum, specifically the splenium. Similar microbleedings have been reported in cases concerning high-altitute exposure, related to hypoxemia and injury of the Blood-Brain Barrier. The observed microbleedings are reminiscent of axonal injury, but head trauma is ruled out. Two distinct pathogeneses are hypothesized: demyelination and disruption of the Blood-Brain Barrier. Both pathogeneses are related to hypoxia caused by SARS-CoV-2 (COVID-19-associated Diffuse Leukoencephalopathy and Microhemorrhages, RSNA Radiology, 21 May 2020).
2.1.6 Acute Necrotizing Encephalopathy (ANE)
A first report of presumptive COVID-19 associated acute necrotizing encephalopathy (ANE) presents one case in which testing for the presence of SARS-CoV-2 in CSF could not be performed. CT images reveal symmetric hypoattenuation within the bilateral medial thalami; brain MRI imaging reveals hemorrhagic rim enhancing lesions within the bilateral thalami, medial temporal lobes and subinsular regions. Basilar arteries and proximal posterior arteries are normal, while axial venogram demonstrates normal functioning of the cerebral venous vasculature and internal cerebral veins. ANE is a rare complication of influenza and other viral infections, being attributed to intracranial cytokine storms resulting in Blood-Brain Barrier damage, but in absence of direct viral invasion of the brain or parainfectious demyelination (COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features, RSNA Public Health Emergency Collection, Radiology 2020 Mar 31: 201187).
A patient with a history of aplastic anemia with intermittent red blood cell and platelet transmission had not received immunosuppression recently. The patient presented with episodes of vacant staring, speech arrest, flexion of both shoulders and a brief tonic clonic seizure. A CT showed early swelling of the brain stem. New lymphopenia was observed. Thrombocytopenia consistent with aplastic anemia was treated with human leukocyte antigen-matched platelets. Repeat head CT showed increased hypodensity and swelling of the brain stem, new cortical and subcortical hypodensity in the occipital lobe and progression of brain stem swelling with pontine hemorrhage and symmetrical hypodensities in the deep grey matter and both amygdalae. CSF showed protein elevation, but normal white blood cell counts. CSF PCR for SARS-CoV-2 was negative; nasopharyngeal swab was positive for SARS-CoV-2.
MRI showed progression of extensive abnormal signal and hemorrhage in a symmetrical distribution within the dorsolateral putamina (situated in the basal ganglia), thalamic nuclei, subinsular regions, splenium of the corpus callosum, cingulate gyri and perirolandic regions. There was reduction of ventriculi, basal cisterns, temporal uncal herniation and moderate celebellar herniation. Severe thrombocytopenia contributed to the hemorrhagic components of encephalopathy. The patient was not lymphopenic before SARS-CoV-2 infection. Testing for interleukins was not possible. Direct invasion (neurotropic) of the CNS by SARS-CoV-2 is unlikely in this case, since the CSF PCR was negative. An immunostorm is a most plausible explanation for this medical picture of ANE (COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia, Neurology Neuroimmunology & Neuroinflammation, 26 May 2020).
2.1.7 ANE successfully treated with steroids
A case of Acute Necrotizing Encephalopathy in a 51-year-old COVID-19 patient without a history of neurological diseases is possibly mediated by antibodies. He presented unresponsive, turning comatose, groaning and showing rhythmic movements of the right upper limb at day 21 of illness, while being weaned off oxygen. Subtle hyperintensities in bilateral thalami were observed. Blood and CSF revealed thrombopenia, lymphopenia and inflammation, CSF albumin-cytological dissociation with increased IgG antibodies and altered Blood-Brain Barrier. MRI showed progressing lesions with diffuse hyperintensity in the thalami, cerebellum, brainstem and supratentorial grey and white matter.
Regions of the fibre network, as ventral hippocampal commissure, brachium of the colliculus and stria medullaris appeared strongly stained. Bilateral distribution of abnormalities to the brainstem, thalami, cerebellum and white matter, hyperintensities and damage to bilateral thalami is distinct in ANE. This is different in clinical pictures of ADEM, which are defined by asymmetrical lesions with ill margins, mainly to be observed in periventricular regions and basal ganglia, with gadolinium enhancement. Early treatment with steroids and polyvalent immunoglobulin has been highly effective. The suspected cause is host response to SARS-CoV-2, associated with IgG targeting a neuronal antigen in fibre tracts. The antibodies are hypothesized to target an autoantigen through molecular mimicry with the virus, while cell destruction, the release of large amounts of autoantigens stimulate self-reactive cells and may lead to self-reactive antibodies. Inflammation contributes to IgG production and alteration of the Blood-Brain Barrier (COVID-19-associated Acute Necrotizing Encephalopathy successfully treated with steroids and polyvalent immunoglobulin with unusual IgG targeting the cerebral fibre network, Postscript Letter, Journal of Neurology, Neurosurgery & Psychiatry, 10 July 2020).
2.1.8 Meningitis/encephalitis associated with SARS-CoV-2 infection of the CNS
A February 2020 report describes a first case of a 24-year-old unconscious patient presenting with suspected meningitis/encephalitis associated with SARS-CoV-2 infection. Neck stiffness and seizures were observed. MRI demonstrated abnormal findings of medial temporal lobe, including hippocampus, suggesting encephalitis. In addition, significant paranasal sinusitis was observed, a finding warranting to pay attention to retrograde synaptic transmission of SARS-CoV-2. While SARS-CoV-2 was not detected in the nasopharyngeal swab, CSF was positive for SARS-CoV-2. CSF lymphocyte count was slightly elevated (pleocytosis). Blood lymphocytes were decreased, white cell count was increased, neutrophils were dominant and C-reactive protein was increased. FLAIR imaging indicated right lateral ventriculitis and encephalitis on the right mesial lobe and hippocampus (A first case of meningitis/encephalitis associated with SARS-CoV-2, International Journal of Infectious Diseases, Vol. 94, May 2020).
In the case of a 41-year-old patient with meningoencephalitis, no RT-PCR of the spinal fluid was taken, but administration of Hydroxychloroquine (HCQ) showed a remarkable improvement (Meningoencephalitis without respiratory failure in a young female with COVID-19 infection in Downtown LA, early April 2020, Brain, Behavior and Immunity, 2020 Jul; 87: 33).
2.1.9 ADEM: 2 cases of improvement after administration of Methylprednisolone or Dexamethasone
Acute disseminated encephalomyelitis (ADEM) is an autoimmune disease of the nervous system, a rare disease that often occurs after viral infections and that mainly affects children. However, cases of ADEM affecting adults following SARS-CoV-2 infection are reported. In one case involving a 64-year-old, the patient reported a loss of smell and taste, rapidly evolving into anosmia and ageusia, followed by bilateral vision impairment associated with sensory loss on the right leg. Relative afferent pupillary defect was detected and visual field tests showed defects bilaterally. Furthermore, irritability, headache, right abdominal sensory level and left-sided lower limb hyper-reflexia were detected. Brain and spine MRI revealed lesions of the brain, associated with one lesion at the eighth thoracic vertebra (T8) and bilateral optic nerve enhancement. CSF showed lymphotic pleocytosis, mainly presented by CD3+CD4+-T-cells and mild proteinorrachia (elevated proteins in CSF). Identical immunoglobulin G oligoclonal bands were present in CSF and serum. SARS-CoV-2 was detected in CSF. Serum revealed anti-SARS-CoV-2 IgG. The serum was negative for antiaquaporin-4 (AQ4) antibody and antimyelin oligodendrocyte glycoprotein (MOG), making a Neuromyelitis optica spectrum syndrome less likely. Treatment with methylprednisolone associated with IV immunoglobulins progressively improved the symptoms associated with ADEM (Acute disseminated encephalomyelitis after SARS-CoV-2 infection, Neuroimmunology & Neuroinflammation, 1 June 2020).
A 54-year-old presented with an episode of lost consciousness and prolonged anosmia and ageusia. RT-PCR for SARS-CoV-2 was positive. X-ray revealed interstitial pneumonia. Blood tests showed moderate lymphocytopenia and mild elevation of inflammatory indices (white blood cells, C-reactive protein, Fibrinogen). Upon sudden deterioration, a Blood Gas test was performed to reveal severe hypoxia. An EEG revealed two seizures started from the right frontotemporal region, diffusing in homologous contralateral hemisphere.
On MRI, multiple hyperintense lesions of the periventricular white matter were observed, without restriction or diffusion nor enhancement. Similar lesions were found in the bulbo-medullary junction, the cervical and spinal cord. CSF RT-PCR for SARS-CoV-2 returned negative.
In this case, the demyelination is thought to be sustained by a delayed immune response after the viremia. Systemic Inflammatory Response Syndromes (SIRS) or SIRS-like syndromes in SARS-CoV-2 patients can occur due to a cytokine storm, in which IL-1, IL-6 and Tumor Necrosis Factor-alpha (TNF-α) may be responsible for activation of glial cells, with subsequant demyelination. It is hypothesized that pneumonia with hypoxia leads to an increased anaerobic metabolism that triggers neurological damage. The virus could alternatively trigger the production of antibodies against glial cells, post-infection, which is associated with Guillain-Barré. Administration of Dexamethasone allowed a progressive recovery of the pulmonary impairment (SARS-CoV-2 can induce brain and spine demyelating lesions, Acta Neurochirurgica 162, 1491-1494 (2020), 4 May 2020).
Non-typical ADEM: axonal injury associated with microthrombosis in the brain
Distinct from a classic ADEM, a non-typical ADEM describes the case of a 71-year-old, whose autopsy shows mild brain swelling and hemorrhagic lesions disseminated throughout the white matter of the cerebral hemisphere. One day before SARS-CoV-2 diagnosis, the patient developed acute kidney injury, likely secondary to shock state and respiratory failure and contrast administration. Levels of C-reactive protein, ferritin and IL-6 were significantly elevated. The brain lesions consisted of foci of intraparenchymal blood disrupting the white matter, with macrophages at the periphery of the lesions. Generalized reactive gliosis was widespread in the white matter.
Damaged axons were highlighted at the periphery of the hemorrhages. A loss of myelin was identified, with macrophages and fragmented axonal processes within the lesions and oligodendrocyte apoptosis surrounding the lesions. Nearby hemorrhagic lesions, the tissue was relatively preserved. Subtle areas of subcortical white matter were seen with a variable perivenular distribution. Perivascular infiltrates were revealed to be macrophages and corresponding myelin loss was visible. The lesions showed a range of axonal injury, up to moderate axonal injury. Additional white matter lesions showed destructive lesions with central fibrin associated with forced out red blood cells, radiating loss of myelin around vessels. Axonal injury was marked at these microscopically identified lesions.
Microscopic cortical infarcts were identified with astrogliosis surrounding the infarcts. Necrotized neurons were scattered in the neocortex, CA1 hippocampal region and Purkinje cells in the cerebellum, indicative of hypoxic-ischemic injury. Scant perivascular T cells were seen, but no activation of B cells was observed. Immunostaining of the brainstem highlighted perivascular macrophages associated with arteriosclerosis. The white matter lesions are hypothesized to be vascular. Microscopic neocortical infarctions are likely associated with microthromboembolism due to SARS-CoV-2 infection, with a role for the ACE2-receptor as a mechanism for the injury (Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology, Acta Neuropathologica (2020): 140:1-6).
2.2 Markers for severe infection
Patients with severe infection had higher white blood cell counts, neutrophil counts, lower blood platelet counts, lower lymphocyte counts, increased C-reactive protein levels, high D-dimer levels, MOF, increased Lactate Dehydrogenase, Alanine Aminotransferase and Aspartate Aminotransferase levels, increased urea nitrogen, elevated creatinine levels and increased creatinine kinase levels. Patients with skeletal muscle injury had decreased lymphocyte counts and serious liver injury as well as kidney injury (Neurologic Manifestions of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China, JAMA Neurology, April 10, 2020). Neurotropic infection of the Central Nervous System (direct virus invasion of the nervous system) is to be determined by CSF PCR. Postinfectious immune-mediated neurological disorders (such as ADEM and Guillain-Barré) can be distinguished from encephalitis by the absence of CSF pleocytosis, as well as elevated CSF protein.
3. Mechanisms
3.1 Penetration or avoidance of the Blood Brain Barrier and Blood Nerve Barrier
The ACE2-receptor (angiotensin-converting enzyme 2-receptor), is the host receptor for SARS-CoV-2. The binding of SARS-CoV-2 comprises S-glycoprotein cleavage by Furin and priming by transmembrane protease serine 2, TMPRSS2, located in the cell membrane. ACE2 has at least two distinct functions. In the RAS, the Renin-Angiotensin-Aldosterone System that regulates blood pressure, it cleaves Angiotensin I to Ang 1-9 and Angiotensin II to Ang 1-7, which functions as a vasodilator peptide. ACE2 also regulates the absorbance of aminon acids in the endothelium of the gut. ACE2 is found in the subfornical organ (SFO) in the brain, an area that regulates the cardiovascular system through fluid balance and hormone secretion. The SFO lacks the protection of the Blood Brain Barrier, which is why circulating peptides can reach the SFO.
The Blood Brain Barrier (BBB) protects the Central Nervous System (brain and spinal cord) from direct interaction with the circulatory system. The BB consists of endothelial cells, a basement membrane, astrocytes and mural cells. Two main immune cells that interact with the CNS are perivascular macrophages and microglial cells. Blood-borne progenitors cross the BBB (The Blood-Brain Barrier, Cold Spring Harbor Perspectives in Biology, 2015 Jan; 7(1)). The targeting of immune cells constitutes immune-mediated inflammatory mechanisms that drive neurological manifestations. Viral replication and the release of cytokines increase the permeability of the BBB (Potential of SARS-CoV-2 to cause CNS infection: Biologic Fundamental and Clinical Experience, Frontiers in Neurology, 18 June 2020).
SARS-CoVs are primarily involved in endotheliitis. This is associated with SARS-CoV's potential to directly infect the CNS by dysregulating the BBB though infection of the vascular endothelium. The main route is the ACE2 receptor expressed on endothelial cells. Avoiding the BBB or the Blood Nerve Barrier (BNB) in order to access the CNS is also possible when a virus enters dorsal root ganglia and autonomic ganglia (The neurology of COVID-19 revisited: A proposal from the Environmental Neurology Specialty Group of the World Federation of Neurology to implement international neurological registries, Journal of Neurological Sciences 414 (2020) 116884).
3.2 Dissemination through neural olfactory connections
It is hypothesized that CNS invasion by SARS-CoV-2 affects respiratory function through damage of the medullary cardiorespiratory center. In transgenic rodent models, SARS-CoV was found to spread through the olfactory pathway to subcortical and cortical brain regions. The brainstem being infected by SARS-CoV sheds light on the possibility that the primary afferents of cranial nerves are involved in the invasion. Since no SARS-CoV has been detected outside the neurons of infected brain specimens, it seems likely that invasion of the CNS from peripheral nerves comprises synaptic connections between neural circuits. This should not be confused with central glial substance and cerebrospinal fluid (CSF) being possible routes for SARS-CoV-infection, since both reveal high ACE2 levels. SARS-CoV-2 could enter the olfactory pathway by infecting epithelial cells in the mucosa. Olfactory axons, the output from olfactory receptors, cross the cribriform plate in the ethmoid bone to end in the olfactory bulb and rhinencephalon. This mechanism, in which a virus infects neurons in the periphery in order to use axonal transport to invade the CNS, is called retrograde (axonal) transport. Noteworthy is the finding that high amounts of ACE2 and TMPRSS2 are expressed in the sustentacular cells of the olfactory epithelium.
Olfactory bulb-hypothalamus-hippocampus-thalamus-cortical-PAG-amygdala
The olfactory bulb projects to the olfactory nucleus, olfactory tubercle, amygdala, piriform cortex, peri-amygdaloid cortex, insula and the anterior end of the parahippocampal gyrus (Anatomy of the olfactory nerves, Nerves and nerve injuries, Chapter 18, Vol. 1: 2015, p. 273-276). The entorhinal cortex of the olfactory complex supplies afferent fibers along the entire length of the hippocampus. The olfactory system sends fibers directly to cortical regions, such as the frontal lobe, without synapsing in the thalamus (Cranial Nerve I: Olfactory Nerve, Textbook of Clinical Neurology, 2007, p. 99-112). The amygdala is part of a broad brain complex that includes the hypothalamus, hippocampus, orbitofrontal cortex and periaqueductal grey matter (PAG). The amygdala has reciprocal connections with the hypothalamus through the fornix and stria terminalis and with the PAG. It receives projections from the prefrontal cortex (Amygdala and hypothalamus: historical overview with focus on aggression, Neurosurgery Vol. 85, Issue 1, July 2019).
The corticomedial (middle of the cortex situated) amygdala is connected to the anterior preoptic and ventromedial nucleus of the hypothalamus (note: the POA contains PGD2 (prostaglandin) synthase-expressing neurons). The central nucleus of the amygdala is connected to the lateral hypothalamus (see Grey's Anatomy 2nd edition, 2008 and 2010). The piriform cortex contains feedback circuits within the cortex and centrifugal axons to the ipsilateral (same side) olfactory bulb, as well as connections to the contralateral (opposite side) olfactory pathway (Olfaction and Taste, Architecture of the Olfactory Bulb, in: The Senses: a comprehensive reference vol. 4, 2008). Notably, ACE2 is found to be highly expressed in the piriform cortex, as well as in hypothalamic nuclei, ventricles, substantia nigra, amygdala, hippocampi and the frontal cortex (abundant information on ACE2 in the brain is found in the 2008 review "Angiotensin-converting enzyme 2 in the brain: properties and future directions", Journal of Neurochemistry, 2008 Dec; 107(6)).
Nervus trigeminus and its neural pathway to the autonomous system
The largest cranial nerve is the trigeminal nerve (nervus trigeminus, V (= fifth) ), extended into mandibular, maxillary and opthalmic branches. It serves as a sensory and motor nerve. The trigeminal nuclei are located in the brain stem. Trigeminal neurons receive sensory information from facial mucosa. The afferent sensory fibers of the trigeminal nerve originate from cell bodies in the Gasserian ganglion. The sensory primary afferents synapse at the Trigeminal Brainstem Nuclear Complex (VBNC) that extends through the brainstem. The fibers terminate in the ventral posteromedial nucleus (VPM) of the thalamus.
Due to a lack of autopsy specimens, viral replication of SARS-CoV-2 in the CNS cannot be confirmed. That is no reason to not raise awareness on the CNS and PNS invasive potential of SARS-CoV-2. Aside from direct neuroinvasion of the CNS, neurological manifestations evoked by inflammation and coagulation disorders (thrombosis and embolism) should be monitored closely. In this review, I will elaborate on the neuroinvasive potential of coronaviruses, neurological manifestations and mechanisms behind CoV-CNS infection. What is the point in drawing a distinction between neurological manifestations that start with direct invasion of the CNS or CNS manifestations mediated by inflammation in the periphery (outside of the CNS)? It is of relevance in respect of therapeutic options and timing of medical intervention.
1. On the neuroinvasive potential of coronaviruses (2016-2020);
2. Neurological manifestations concerning viral infection;
2.1 Manifestations of the nervous system in SARS-CoV-2 patients;
2.1.1 Encephalopathy;
2.1.2 MRI-findings in absence of specific CSF findings: unspecific encephalitis;
2.1.3 Unusual microbleeds;
2.1.4 Systemic hyperinflammatory CNS dysfunction;
2.1.5 Leukoencephalopathy and microhemorrhages (punctate bleedings);
2.1.6 Acute Necrotizing Encephalopathy (ANE);
2.1.7 ANE successfully treated with steroids;
2.1.8 Meningitis/encephalitis associated with SARS-CoV-2 infection of the Nervous System;
2.1.9 ADEM (Acute Disseminated encephalomyelitis): 2 cases of improvement after Methylprednisolone or Dexamethasone;
2.2 Markers for severe infection;
3 Mechanisms
3.1 Penetration or avoidance of the Blood Brain Barrier and Blood Nerve Barrier;
3.2 Dissemination through neural olfactory (smell and taste) connections
1. On the neuroinvasive potential of coronaviruses (2016-2020)
Like respiratory viruses in general, SARS-CoVs can cause damage to the central nervous system. Coronaviruses can induce encephalitis, as accumulation of interleukin-6 increases the permeability of the blood-brain barrier. The rapid replication of SARS-CoV-2 is a risk factor for initiating overreaction of the human immune system; viral meningitis can occur as a consequence (Human Coronaviruses and other respiratory viruses: Underestimated opportunistic pathogens of the Central Nervous System?, Viruses 2020, 12 (1), 14, published December 20, 2019). In a young patient group with CoV, a slight accumulation of IL-6, IL-8 and MCP-1 in the brain fluid was observed. MCP-1 is involved in initiating inflammatory responses in the brain (Coronavirus infections in the Central Nervous System and respiratory tract show distinct features in hospitalized children, Intervirology 2016, vol. 59, no. 3, published in February 2017).
In this 2016 study, a distinction was drawn between Coronavirus-CNS infection (CoV-CNS) and CoV-respiratory tract infection. The serum level of Granulocyte macrophage colony-stimulating factor (GM-CSF) was higher in CoV-CNS infected patients. GM-CSF has proinflammatory properties and plays a role in autoimmune encephalopathy. Levels of IL-6, IL-8, MCP-1 and GM-CSF were higher in cerebrospinal fluid samples of the CoV-CNS patient group. Lymphocyte and eosinophil counts were reduced in the CoV-CNS group, whereas CoV-respitatory tract patients had a significantly lower neutrophil cell count. The monocyte count in CoV-CNS was elevated. Notably, the serum level of Granulocyte colony-stimulating factor (G-CSF) was significantly elevated in CoV-CNS and CoV-respiratory infection alike.
Autopsies performed during the SARS-CoV-1 epidemic revealed viral RNA in the cytoplasm of hypothalamic and cerebral cortical neurons, as well as brain edema and focal neuronal degeneration and neuronal necrosis, extensive glial cell hyperplasia and cellular infiltrates. No demyelination was reported. Interferon-gamma was expressed in glia, infiltration of CD68+ macrophages and CD3+ T-cells was observed in brain neurons and glia (The neurology of COVID-19 revisited: A proposal from the Environmental Neurology Specialty Group of the World Federation of Neurology to implement international neurological registries, Journal of Neurological Sciences 414 (2020) 116884).
In ACE2 transgenic mice models, respiratory failure has been attributed to medullary infection with SARS-CoV. While little cellular infiltration was observed, the entry for viral infection of the brain was the olfactory nerve. One report on COVID-19 encephalitis reveals hemorrhagic rim enhancing lesions within the thalami, medial temporal lobes and subinsula. The potential for viral-induced vasculitis via brain endothelial ACE2-receptors increases the risk of cerebrovascular disease (COVID-19 and the nervous system, Journal of Neurovirology, 2020 May 23).

2. Neurological manifestations concerning viral infection
There are at least three categories of neurological manifestations associated with viral infection. Encephalopathy, inflammatory encephalitis, hemorrhagic and ischemic stroke are complications of systemic diseases, such as Multi Organ Failure, inflammation and coagulation. Direct viral invasion of the CNS results in encephalitis, meningitis and endotheliitis associated with cell necrosis and dysfunction. Acute Disseminated Encephalomyelitis (ADEM), Acute Necrotizing Encephalopathy (ANE), Guillain-Barré Syndrome and Kawasaki-like manifestations are immune-mediated post-infectious manifestations.
2.1 Manifestations of the nervous system in SARS-CoV-2 patients
In a case study involving 214 patients with SARS-CoV-2, neurologic symptoms were seen in 36,4% of patients. Mean age of patients was 52 years. Of all reported patients with nervous system manifestations, 24,8% had CNS manifestations, 8,9% had Peripheral Nervous System manifestations and 10,7% had skeletal muscle injury. Typical Peripheral Nervous System symptoms are anosmia and ageusia (loss of smell and taste). Notably, 58,9% of patients with CNS manifestations had nonsevere infection. Neurologic manifestations occurred within 1-2 days of the infection. 2 patients were admitted to the hospital with SARS-CoV-2-induced hemiparese, of whom none had fever, cough or diarrhea. Of CNS manifestions, headache, impaired consciousness, acute cerebrovascular disease, coma, delirium, ischemic stroke and cerebral hemorrhage were reported.
2.1.1 Encephalopathy
In a study concerning 58 patients, 69% had agitation, 67% had diffusive corticospinal tract signs and 33% had dysexecutive syndrome consisting of attention difficulties, disorientation and poorly organized response movements. In 8 patients, enhancement in leptomeningeal spaces was noted; in 11 patients, bilateral frontotemporal hypoperfusion was noted. 1 of 8 patients had diffuse bifrontal slowing consistent with encephalopathy; in 2 patients, oligoclonal bands were present, protein and IgG levels were elevated in 1 patient. RT-PCR arrays of the Cerebrospinal Fluid (CSF) were negative for SARS-CoV-2. Pleocytosis was not observed in any of the cases. This study concludes that ARDS due to SARS-CoV-2 infection was associated with encephalopathy, agitation, confusion and corticospinal tract signs. However, no conclusions can be drawn with regards to inflammation-mediated encephalopathy, as no cytokine arrays were performed (Neurologic Features in Severe SARS-CoV-2 Infection, NEJM, 4 June 2020).
2.1.2 MRI findings in absence of specific CSF findings: unspecific encephalitis
A study investigating 50 patients reports that the most common finding was cortical signal abnormalities on Fluid-Attenuated Inversion Recovery (FLAIR). In 3 patients, accompanying subcortical and deep white matter signal abnormalities were present; abnormalities in the frontal lobe were present in 4 patients; parietal lobe in 3; occipital lobe in 4; temporal lobe in 1; insular cortex in 3 and cingulate gyrus in 3 patients. CSF array of 5 patients revealed total elevated protein in 4 patients. Cell count, albumin, glucose levels and IgG Index were within normal range, no oligoclonal bands were observed. Acute intracranial findings in the absence of cortical signal abnormality included 1 patient with acute transverse sinus thrombosis and 1 patient with acute infarction in the right middle cerebral artery territory. Of 2 cases without intracranial findings, elevated protein was found in the CSF. The main differential diagnosis of these findings is infectious or autoimmune encephalitis, seizure, hypoxia and hypoglycemia. The cases of bilateral frontal involvement may have hypoexia as underlying pathogenesis, as ARDS and frontotemporal perfusion are associated factors. Cortical microhemorrhage and breakdown of the Blood-Brain Barrier accompanied by hypoxia are thought to result in the observed imaging pattern. Overall, no conclusions can be drawn with regards to viral or immunity-mediated encephalitis (Brain MRI Findings in Patients in the ICU with COVID-19 Infection, RSNA Radiology, 8 May 2020).
2.1.3 Unusual microbleeds
MR images of 9 patients with a common pattern of unusual findings are reported. All patients suffered from severe hypoxemia secondary to ARDS, with a delayed recovery of consciousness after sedation. None of the patients were reported to have Diffuse Intravascular Coagulation (DIC); all patients presented a hyperfibrinemic state as well as septic or inflammatory coagulation. Microbleeds were observed in unusual distribution with a specific tendency for the corpus callosum. Other locations of microbleeds were the posterior or anterior limbs of internal capsule and middle cerebellar peduncles. In the majority of the patients, subcortical regions were affected. These findings are assessed to be distinct from hypertension and amyloid angiopathy. The involvement of the corpus callosum is inconsistent with hypertension and amyloid angiopathy; short episodes of hypertension occurred in 2 of 9 patients, who were successfully treated with antihypertensives. It is hypothesized that direct damage to the endothelium and vessels could be explanatory, as direct interaction between SARS-CoV-2 and the ACE2-receptor could lead to damage of the Blood-Brain Barrier and bleeding within the brain tissue. Some of the lesions observed on MR imaging were reported to have a lineal shape resembling a vessel, which could represent microthrombi within vessels, consistent with hypercoagulation disorders and microthrombi in pulmonary vessels of other patients. Lastly, diffuse axonal injury or lipid embolism are explored as possible explanations (Unusual Microbleeds in Brain MRI of COVID-19 Patients, Journal of Neuroimaging, 8 July 2020).
2.1.4 Systemic hyperinflammatory CNS dysfunction
1 patient without comorbidities presented with left-sided paresthesias, a 1-day history of headache and ipsilateral paresis progressing within 12 hours to confusion and agitation. CSF showed lymphotic pleocytosis and increased proteins. PCR of SARS-CoV-2 in CSF returned negative, but positive in the nasopharyngeal swab. A second patient presented with agitation, difficulties naming objects, temporospatial disorientation and confusion. CSF showed lymphotic pleocytosis and increased proteins. In both patients, IL-6 was elevated, in one patient IL-1β was significantly elevated. In addition, CSF showed elevated levels of ACE in both patients. It is hypothesized that these cases of encephalitis are triggered by a cytokine storm. Treatments targeting IL-6 (tocilizumab) and IL-1 (anakinra) could be of benefit to treat CNS dysfunction (Increased CSF levels of IL-1β, IL-6 and ACE in SARS-CoV-2-associated encephalitis, Neuroimmunology & Neuroinflammation, 1 July 2020).
2.1.5 Leukoencephalopathy and microhemorrhages
11 patients were indicated for brain MRI for persistently depressed mental status. Brainstem reflexes were preserved, response in extremities was diminished. None of the patients had overt Disseminated Intravascular Coagulation. CSF was available in only 1 patient and was negative for infectious or inflammatory meningitis and encephalitis and was negative for SARS-CoV-2 on RT-PCR array. Of 11 patients, 4 patients presented with diffuse leukoencephalopathy, 1 with microhemorrhages and 6 with both microhemorrhages and leukoencephalopathy. Patients with leukoencephalopathy had symmetric hyperintensities involving bilateral deep and subcortical white matter. Abnormalities were observed to extend from the precentral gyrus down to the centrum semiovale and corona radiata. At the temporal and occipital horns, the posterior cerebral white matter was involved in all patients, notably more than the anterior white matter. The deep grey nuclei were spared from leukoencephalopathy. Apart from the pre-central gyrus and occipital lobes, the juxtacortical white matter was spared from leukoencephalopathy. These findings are reported to be consistent with Delayed Posthypopoxic Leukoencephalopathy (DPHL), occurring 10-14 days after hypoxic insult and similar to a pattern in carbon monoxide poisoning victims. The sparing of juxtacortical white matter and deep grey nuclei rules out acute hypoxic ischemia. DPHL is likely related to oligodendroglial cell death and subsequent demyelination. Observed mild restricted diffusion in this study can be related to acute demyelination. Possible etiologies for the observed leukoencephalopathy are sepsis-associated, post-infectious demyelating or hemorrhagic encephalitis and posterior reversible encephalopathy syndrome.
Punctate microhemorrhages were seen in the juxtacortical white matter and corpus callosum, specifically the splenium. Similar microbleedings have been reported in cases concerning high-altitute exposure, related to hypoxemia and injury of the Blood-Brain Barrier. The observed microbleedings are reminiscent of axonal injury, but head trauma is ruled out. Two distinct pathogeneses are hypothesized: demyelination and disruption of the Blood-Brain Barrier. Both pathogeneses are related to hypoxia caused by SARS-CoV-2 (COVID-19-associated Diffuse Leukoencephalopathy and Microhemorrhages, RSNA Radiology, 21 May 2020).
2.1.6 Acute Necrotizing Encephalopathy (ANE)
A first report of presumptive COVID-19 associated acute necrotizing encephalopathy (ANE) presents one case in which testing for the presence of SARS-CoV-2 in CSF could not be performed. CT images reveal symmetric hypoattenuation within the bilateral medial thalami; brain MRI imaging reveals hemorrhagic rim enhancing lesions within the bilateral thalami, medial temporal lobes and subinsular regions. Basilar arteries and proximal posterior arteries are normal, while axial venogram demonstrates normal functioning of the cerebral venous vasculature and internal cerebral veins. ANE is a rare complication of influenza and other viral infections, being attributed to intracranial cytokine storms resulting in Blood-Brain Barrier damage, but in absence of direct viral invasion of the brain or parainfectious demyelination (COVID-19-associated Acute Hemorrhagic Necrotizing Encephalopathy: CT and MRI Features, RSNA Public Health Emergency Collection, Radiology 2020 Mar 31: 201187).
A patient with a history of aplastic anemia with intermittent red blood cell and platelet transmission had not received immunosuppression recently. The patient presented with episodes of vacant staring, speech arrest, flexion of both shoulders and a brief tonic clonic seizure. A CT showed early swelling of the brain stem. New lymphopenia was observed. Thrombocytopenia consistent with aplastic anemia was treated with human leukocyte antigen-matched platelets. Repeat head CT showed increased hypodensity and swelling of the brain stem, new cortical and subcortical hypodensity in the occipital lobe and progression of brain stem swelling with pontine hemorrhage and symmetrical hypodensities in the deep grey matter and both amygdalae. CSF showed protein elevation, but normal white blood cell counts. CSF PCR for SARS-CoV-2 was negative; nasopharyngeal swab was positive for SARS-CoV-2.
MRI showed progression of extensive abnormal signal and hemorrhage in a symmetrical distribution within the dorsolateral putamina (situated in the basal ganglia), thalamic nuclei, subinsular regions, splenium of the corpus callosum, cingulate gyri and perirolandic regions. There was reduction of ventriculi, basal cisterns, temporal uncal herniation and moderate celebellar herniation. Severe thrombocytopenia contributed to the hemorrhagic components of encephalopathy. The patient was not lymphopenic before SARS-CoV-2 infection. Testing for interleukins was not possible. Direct invasion (neurotropic) of the CNS by SARS-CoV-2 is unlikely in this case, since the CSF PCR was negative. An immunostorm is a most plausible explanation for this medical picture of ANE (COVID-19-related acute necrotizing encephalopathy with brain stem involvement in a patient with aplastic anemia, Neurology Neuroimmunology & Neuroinflammation, 26 May 2020).
2.1.7 ANE successfully treated with steroids
A case of Acute Necrotizing Encephalopathy in a 51-year-old COVID-19 patient without a history of neurological diseases is possibly mediated by antibodies. He presented unresponsive, turning comatose, groaning and showing rhythmic movements of the right upper limb at day 21 of illness, while being weaned off oxygen. Subtle hyperintensities in bilateral thalami were observed. Blood and CSF revealed thrombopenia, lymphopenia and inflammation, CSF albumin-cytological dissociation with increased IgG antibodies and altered Blood-Brain Barrier. MRI showed progressing lesions with diffuse hyperintensity in the thalami, cerebellum, brainstem and supratentorial grey and white matter.
Regions of the fibre network, as ventral hippocampal commissure, brachium of the colliculus and stria medullaris appeared strongly stained. Bilateral distribution of abnormalities to the brainstem, thalami, cerebellum and white matter, hyperintensities and damage to bilateral thalami is distinct in ANE. This is different in clinical pictures of ADEM, which are defined by asymmetrical lesions with ill margins, mainly to be observed in periventricular regions and basal ganglia, with gadolinium enhancement. Early treatment with steroids and polyvalent immunoglobulin has been highly effective. The suspected cause is host response to SARS-CoV-2, associated with IgG targeting a neuronal antigen in fibre tracts. The antibodies are hypothesized to target an autoantigen through molecular mimicry with the virus, while cell destruction, the release of large amounts of autoantigens stimulate self-reactive cells and may lead to self-reactive antibodies. Inflammation contributes to IgG production and alteration of the Blood-Brain Barrier (COVID-19-associated Acute Necrotizing Encephalopathy successfully treated with steroids and polyvalent immunoglobulin with unusual IgG targeting the cerebral fibre network, Postscript Letter, Journal of Neurology, Neurosurgery & Psychiatry, 10 July 2020).
2.1.8 Meningitis/encephalitis associated with SARS-CoV-2 infection of the CNS
A February 2020 report describes a first case of a 24-year-old unconscious patient presenting with suspected meningitis/encephalitis associated with SARS-CoV-2 infection. Neck stiffness and seizures were observed. MRI demonstrated abnormal findings of medial temporal lobe, including hippocampus, suggesting encephalitis. In addition, significant paranasal sinusitis was observed, a finding warranting to pay attention to retrograde synaptic transmission of SARS-CoV-2. While SARS-CoV-2 was not detected in the nasopharyngeal swab, CSF was positive for SARS-CoV-2. CSF lymphocyte count was slightly elevated (pleocytosis). Blood lymphocytes were decreased, white cell count was increased, neutrophils were dominant and C-reactive protein was increased. FLAIR imaging indicated right lateral ventriculitis and encephalitis on the right mesial lobe and hippocampus (A first case of meningitis/encephalitis associated with SARS-CoV-2, International Journal of Infectious Diseases, Vol. 94, May 2020).
In the case of a 41-year-old patient with meningoencephalitis, no RT-PCR of the spinal fluid was taken, but administration of Hydroxychloroquine (HCQ) showed a remarkable improvement (Meningoencephalitis without respiratory failure in a young female with COVID-19 infection in Downtown LA, early April 2020, Brain, Behavior and Immunity, 2020 Jul; 87: 33).
2.1.9 ADEM: 2 cases of improvement after administration of Methylprednisolone or Dexamethasone
Acute disseminated encephalomyelitis (ADEM) is an autoimmune disease of the nervous system, a rare disease that often occurs after viral infections and that mainly affects children. However, cases of ADEM affecting adults following SARS-CoV-2 infection are reported. In one case involving a 64-year-old, the patient reported a loss of smell and taste, rapidly evolving into anosmia and ageusia, followed by bilateral vision impairment associated with sensory loss on the right leg. Relative afferent pupillary defect was detected and visual field tests showed defects bilaterally. Furthermore, irritability, headache, right abdominal sensory level and left-sided lower limb hyper-reflexia were detected. Brain and spine MRI revealed lesions of the brain, associated with one lesion at the eighth thoracic vertebra (T8) and bilateral optic nerve enhancement. CSF showed lymphotic pleocytosis, mainly presented by CD3+CD4+-T-cells and mild proteinorrachia (elevated proteins in CSF). Identical immunoglobulin G oligoclonal bands were present in CSF and serum. SARS-CoV-2 was detected in CSF. Serum revealed anti-SARS-CoV-2 IgG. The serum was negative for antiaquaporin-4 (AQ4) antibody and antimyelin oligodendrocyte glycoprotein (MOG), making a Neuromyelitis optica spectrum syndrome less likely. Treatment with methylprednisolone associated with IV immunoglobulins progressively improved the symptoms associated with ADEM (Acute disseminated encephalomyelitis after SARS-CoV-2 infection, Neuroimmunology & Neuroinflammation, 1 June 2020).
A 54-year-old presented with an episode of lost consciousness and prolonged anosmia and ageusia. RT-PCR for SARS-CoV-2 was positive. X-ray revealed interstitial pneumonia. Blood tests showed moderate lymphocytopenia and mild elevation of inflammatory indices (white blood cells, C-reactive protein, Fibrinogen). Upon sudden deterioration, a Blood Gas test was performed to reveal severe hypoxia. An EEG revealed two seizures started from the right frontotemporal region, diffusing in homologous contralateral hemisphere.
On MRI, multiple hyperintense lesions of the periventricular white matter were observed, without restriction or diffusion nor enhancement. Similar lesions were found in the bulbo-medullary junction, the cervical and spinal cord. CSF RT-PCR for SARS-CoV-2 returned negative.
In this case, the demyelination is thought to be sustained by a delayed immune response after the viremia. Systemic Inflammatory Response Syndromes (SIRS) or SIRS-like syndromes in SARS-CoV-2 patients can occur due to a cytokine storm, in which IL-1, IL-6 and Tumor Necrosis Factor-alpha (TNF-α) may be responsible for activation of glial cells, with subsequant demyelination. It is hypothesized that pneumonia with hypoxia leads to an increased anaerobic metabolism that triggers neurological damage. The virus could alternatively trigger the production of antibodies against glial cells, post-infection, which is associated with Guillain-Barré. Administration of Dexamethasone allowed a progressive recovery of the pulmonary impairment (SARS-CoV-2 can induce brain and spine demyelating lesions, Acta Neurochirurgica 162, 1491-1494 (2020), 4 May 2020).
Non-typical ADEM: axonal injury associated with microthrombosis in the brain
Distinct from a classic ADEM, a non-typical ADEM describes the case of a 71-year-old, whose autopsy shows mild brain swelling and hemorrhagic lesions disseminated throughout the white matter of the cerebral hemisphere. One day before SARS-CoV-2 diagnosis, the patient developed acute kidney injury, likely secondary to shock state and respiratory failure and contrast administration. Levels of C-reactive protein, ferritin and IL-6 were significantly elevated. The brain lesions consisted of foci of intraparenchymal blood disrupting the white matter, with macrophages at the periphery of the lesions. Generalized reactive gliosis was widespread in the white matter.
Damaged axons were highlighted at the periphery of the hemorrhages. A loss of myelin was identified, with macrophages and fragmented axonal processes within the lesions and oligodendrocyte apoptosis surrounding the lesions. Nearby hemorrhagic lesions, the tissue was relatively preserved. Subtle areas of subcortical white matter were seen with a variable perivenular distribution. Perivascular infiltrates were revealed to be macrophages and corresponding myelin loss was visible. The lesions showed a range of axonal injury, up to moderate axonal injury. Additional white matter lesions showed destructive lesions with central fibrin associated with forced out red blood cells, radiating loss of myelin around vessels. Axonal injury was marked at these microscopically identified lesions.
Microscopic cortical infarcts were identified with astrogliosis surrounding the infarcts. Necrotized neurons were scattered in the neocortex, CA1 hippocampal region and Purkinje cells in the cerebellum, indicative of hypoxic-ischemic injury. Scant perivascular T cells were seen, but no activation of B cells was observed. Immunostaining of the brainstem highlighted perivascular macrophages associated with arteriosclerosis. The white matter lesions are hypothesized to be vascular. Microscopic neocortical infarctions are likely associated with microthromboembolism due to SARS-CoV-2 infection, with a role for the ACE2-receptor as a mechanism for the injury (Neuropathology of COVID-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology, Acta Neuropathologica (2020): 140:1-6).
2.2 Markers for severe infection
Patients with severe infection had higher white blood cell counts, neutrophil counts, lower blood platelet counts, lower lymphocyte counts, increased C-reactive protein levels, high D-dimer levels, MOF, increased Lactate Dehydrogenase, Alanine Aminotransferase and Aspartate Aminotransferase levels, increased urea nitrogen, elevated creatinine levels and increased creatinine kinase levels. Patients with skeletal muscle injury had decreased lymphocyte counts and serious liver injury as well as kidney injury (Neurologic Manifestions of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China, JAMA Neurology, April 10, 2020). Neurotropic infection of the Central Nervous System (direct virus invasion of the nervous system) is to be determined by CSF PCR. Postinfectious immune-mediated neurological disorders (such as ADEM and Guillain-Barré) can be distinguished from encephalitis by the absence of CSF pleocytosis, as well as elevated CSF protein.
 |
| SARS-CoV-2: markers for severe infection and markers for CNS involvement & systemic inflammation |
3. Mechanisms
3.1 Penetration or avoidance of the Blood Brain Barrier and Blood Nerve Barrier
The ACE2-receptor (angiotensin-converting enzyme 2-receptor), is the host receptor for SARS-CoV-2. The binding of SARS-CoV-2 comprises S-glycoprotein cleavage by Furin and priming by transmembrane protease serine 2, TMPRSS2, located in the cell membrane. ACE2 has at least two distinct functions. In the RAS, the Renin-Angiotensin-Aldosterone System that regulates blood pressure, it cleaves Angiotensin I to Ang 1-9 and Angiotensin II to Ang 1-7, which functions as a vasodilator peptide. ACE2 also regulates the absorbance of aminon acids in the endothelium of the gut. ACE2 is found in the subfornical organ (SFO) in the brain, an area that regulates the cardiovascular system through fluid balance and hormone secretion. The SFO lacks the protection of the Blood Brain Barrier, which is why circulating peptides can reach the SFO.
The Blood Brain Barrier (BBB) protects the Central Nervous System (brain and spinal cord) from direct interaction with the circulatory system. The BB consists of endothelial cells, a basement membrane, astrocytes and mural cells. Two main immune cells that interact with the CNS are perivascular macrophages and microglial cells. Blood-borne progenitors cross the BBB (The Blood-Brain Barrier, Cold Spring Harbor Perspectives in Biology, 2015 Jan; 7(1)). The targeting of immune cells constitutes immune-mediated inflammatory mechanisms that drive neurological manifestations. Viral replication and the release of cytokines increase the permeability of the BBB (Potential of SARS-CoV-2 to cause CNS infection: Biologic Fundamental and Clinical Experience, Frontiers in Neurology, 18 June 2020).
SARS-CoVs are primarily involved in endotheliitis. This is associated with SARS-CoV's potential to directly infect the CNS by dysregulating the BBB though infection of the vascular endothelium. The main route is the ACE2 receptor expressed on endothelial cells. Avoiding the BBB or the Blood Nerve Barrier (BNB) in order to access the CNS is also possible when a virus enters dorsal root ganglia and autonomic ganglia (The neurology of COVID-19 revisited: A proposal from the Environmental Neurology Specialty Group of the World Federation of Neurology to implement international neurological registries, Journal of Neurological Sciences 414 (2020) 116884).
3.2 Dissemination through neural olfactory connections
It is hypothesized that CNS invasion by SARS-CoV-2 affects respiratory function through damage of the medullary cardiorespiratory center. In transgenic rodent models, SARS-CoV was found to spread through the olfactory pathway to subcortical and cortical brain regions. The brainstem being infected by SARS-CoV sheds light on the possibility that the primary afferents of cranial nerves are involved in the invasion. Since no SARS-CoV has been detected outside the neurons of infected brain specimens, it seems likely that invasion of the CNS from peripheral nerves comprises synaptic connections between neural circuits. This should not be confused with central glial substance and cerebrospinal fluid (CSF) being possible routes for SARS-CoV-infection, since both reveal high ACE2 levels. SARS-CoV-2 could enter the olfactory pathway by infecting epithelial cells in the mucosa. Olfactory axons, the output from olfactory receptors, cross the cribriform plate in the ethmoid bone to end in the olfactory bulb and rhinencephalon. This mechanism, in which a virus infects neurons in the periphery in order to use axonal transport to invade the CNS, is called retrograde (axonal) transport. Noteworthy is the finding that high amounts of ACE2 and TMPRSS2 are expressed in the sustentacular cells of the olfactory epithelium.
Olfactory bulb-hypothalamus-hippocampus-thalamus-cortical-PAG-amygdala
The olfactory bulb projects to the olfactory nucleus, olfactory tubercle, amygdala, piriform cortex, peri-amygdaloid cortex, insula and the anterior end of the parahippocampal gyrus (Anatomy of the olfactory nerves, Nerves and nerve injuries, Chapter 18, Vol. 1: 2015, p. 273-276). The entorhinal cortex of the olfactory complex supplies afferent fibers along the entire length of the hippocampus. The olfactory system sends fibers directly to cortical regions, such as the frontal lobe, without synapsing in the thalamus (Cranial Nerve I: Olfactory Nerve, Textbook of Clinical Neurology, 2007, p. 99-112). The amygdala is part of a broad brain complex that includes the hypothalamus, hippocampus, orbitofrontal cortex and periaqueductal grey matter (PAG). The amygdala has reciprocal connections with the hypothalamus through the fornix and stria terminalis and with the PAG. It receives projections from the prefrontal cortex (Amygdala and hypothalamus: historical overview with focus on aggression, Neurosurgery Vol. 85, Issue 1, July 2019).
The corticomedial (middle of the cortex situated) amygdala is connected to the anterior preoptic and ventromedial nucleus of the hypothalamus (note: the POA contains PGD2 (prostaglandin) synthase-expressing neurons). The central nucleus of the amygdala is connected to the lateral hypothalamus (see Grey's Anatomy 2nd edition, 2008 and 2010). The piriform cortex contains feedback circuits within the cortex and centrifugal axons to the ipsilateral (same side) olfactory bulb, as well as connections to the contralateral (opposite side) olfactory pathway (Olfaction and Taste, Architecture of the Olfactory Bulb, in: The Senses: a comprehensive reference vol. 4, 2008). Notably, ACE2 is found to be highly expressed in the piriform cortex, as well as in hypothalamic nuclei, ventricles, substantia nigra, amygdala, hippocampi and the frontal cortex (abundant information on ACE2 in the brain is found in the 2008 review "Angiotensin-converting enzyme 2 in the brain: properties and future directions", Journal of Neurochemistry, 2008 Dec; 107(6)).
Nervus trigeminus and its neural pathway to the autonomous system
The largest cranial nerve is the trigeminal nerve (nervus trigeminus, V (= fifth) ), extended into mandibular, maxillary and opthalmic branches. It serves as a sensory and motor nerve. The trigeminal nuclei are located in the brain stem. Trigeminal neurons receive sensory information from facial mucosa. The afferent sensory fibers of the trigeminal nerve originate from cell bodies in the Gasserian ganglion. The sensory primary afferents synapse at the Trigeminal Brainstem Nuclear Complex (VBNC) that extends through the brainstem. The fibers terminate in the ventral posteromedial nucleus (VPM) of the thalamus.
 |
| How the Nervus Trigeminus (trigeminal nerve) is situated |
The solitary tract, located in the medulla, is formed from the ganglion of the vagus nerve, glossopharyngeal and geniculate nerve. The solitary tract nucleus (NST) is described as the visceral nucleus of the brainstem. The nerve fibers departed from the NST synapse in the lateral and paraventricular hypothalamic nuclei, to project to the insula. The nucleus ambiguus (NA) is involved in motor functions of swallowing and speech. Both the NST and the VBNC are situated close to the cardiovascular center in the medulla oblongata, which regulates heart rate through nervous and endocrine control.
 |
| Medulla and pons |
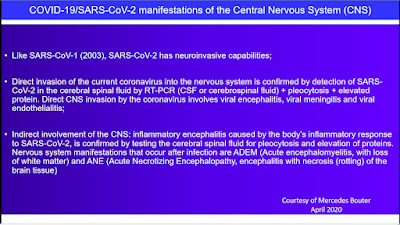
Like SARS-CoV-1 (2003), SARS-CoV-2 has neuroinvasive capabilities. Evidence of CNS invasion is available, but more material from autopsies and biopsies (tissue samples), imaging techniques (CT scans and MRI) will need to be analyzed to specifically assess damage done to the nervous system. In a number of cases there is evidence of direct invasion of the current coronavirus into the nervous system; this is confirmed by detection of SARS-CoV-2 in the cerebral spinal fluid by RT-PCR (CSF or cerebrospinal fluid). Direct CNS invasion by the coronavirus involves viral encephalitis, viral meningitis and viral endothelialitis (inflammation of endothelial tissue, resulting in, among other things, microbleeds in the brain).
In other cases, due to systemic inflammatory mechanisms or a "cytokine storm" in response to SARS-CoV-2 infection, encephalopathy, encephalitis and Kawasaki-like manifestations are caused. Inflammatory encephalitis, an inflammation of the brain caused by the body's inflammatory response to SARS-CoV-2, is confirmed by testing the cerebral spinal fluid for pleocytosis and elevation of proteins. Nervous system manifestations that occur after infection are ADEM (Acute encephalmyelitis, with loss of white matter), ANE (Acute Necrotizing Encephalopathy, encephalitis with necrosis (rotting) of the brain tissue) and Guillain-Barré.
Why the distinction between direct neuroinvasion of SARS-CoV-2 or neurological manifestations caused by inflammatory mechanisms and immunological mechanisms in response to SARS-CoV-2? Direct neuroinvasion, e.g. viral meningitis, should be treated with antiviral therapy. In one case of SARS-CoV-2 meningoencephalitis, a patient was successfully treated with hydroxychloroquine (HCQ). If neurological manifestations are caused by immunological responses, for example Tocilizumab (IL-6 blocker) or Anakinra may provide improvement.
Why the distinction between direct neuroinvasion of SARS-CoV-2 or neurological manifestations caused by inflammatory mechanisms and immunological mechanisms in response to SARS-CoV-2? Direct neuroinvasion, e.g. viral meningitis, should be treated with antiviral therapy. In one case of SARS-CoV-2 meningoencephalitis, a patient was successfully treated with hydroxychloroquine (HCQ). If neurological manifestations are caused by immunological responses, for example Tocilizumab (IL-6 blocker) or Anakinra may provide improvement.
What to expect from COVID-associated CNS manifestations?
In the nearby future, more manifestations involving olfactory tract and retrograde transport will be observed, as well as SARS-CoV-2-associated encephalitis, non-typical ANE and post-COVID Guillain Barré.