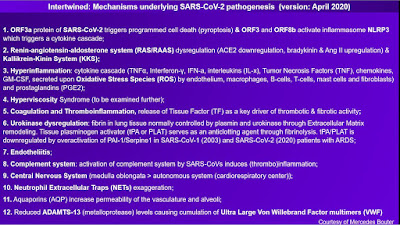
In this "Deterioration series", I will elaborate on the mechanisms underlying the severity of SARS-CoV-2 infection. I made this summary of mechanisms known to contribute to severe complications in COVID-19 patients. There is an ever growing body of knowledge since SARS-CoV-1 (2003), the first SARS-Coronavirus that was associatied with the same mechanisms as are observed in SARS-CoV-2. From this BoK and SARS-CoV-2 reports can be gathered that the following mechanisms are involved:
In this message, I will discuss the influence of SARS-CoV-2 on dysregulation of the Renin-Angiotensin-Aldosterone System (RAS/RAAS). Notably, disruption of ACE2 upregulates Angiotensin II (Ang II). Ang II in its turn increases blood pressure. Actions on the Ang II type I receptor (AT1) adversely affects the
vascular wall and enhances oxidative stress, resulting in endothelial
damage and endothelial cell apoptosis. Oxidative stress increases
expression of plasminogen activator inhibitor type I, resulting in the
recruitment and binding of inflammatory cells to the endothelium, which
leads to inflammation and thrombosis. Aside from ACE2, there is ACE. Bradykinin is a substrate for ACE. Bradykinin has vasodilator and
natriuretic properties. ACE inactivates bradykinin and is therefore
known as kininase II. ACE inhibition increases the level of bradykinin, rendering the vasculature permeable. Thus, reduction of ACE adversely affects degradation of bradykinin, increasing the risk of 'leaking' vessels.
How ACE2 is affected by SARS-CoV-2 pathogens
The spike glycoprotein of SARS-CoV-2 is known to use human (and other mammal, with the exception of some rodents) Angiotensin Converting Enzyme 2-receptors. The ACE2-receptor is found in type II alveolar cells (AT2) of the lungs, esophagus epithelial cells, enterocytes from ileum and colon, nasal cavity, vascular endothelia, renal tissue (kidneys), epithelia of the small intestine, testes and on the epithelial cells of oral mucosa (High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa, International Journal of Oral Science, 24 February 2020), as well as in the brain stem and neural cortex. SARS invades ACE2-enriched cells, only to replicate itself very quickly in order to contract other cells. The infection of type II pneumocytes and release of virus in the respiratory tract with close proximity to the pulmonary capillary bed has been thought to allow systemic spread of virus to distant organs (ACE2 Receptor Expression and SARS Infection Depend on Differentiation of Human Airway Epithelia, Journal of Virology, December 2005).
Uncertainty: is ARDS an adequate classification?
It is yet unclear what exactly constitutes sudden deterioration in critically ill SARS-CoV-2 patients. A sudden deterioration in patients with oxygen deprivation is labelled "Acute Respiratory Distress Syndrome" (ARDS). It is prone to doubt whether ARDS, characterized by bilateral infiltrates, hypoxaemia and dyspnea (Acute Lung Injury and ARDS: Pathophysiology and Treatment, Missouri Medicine, Jul-Aug 2010), is an adequate classification for the pathophysiology associated with SARS-CoV-2 (COVID-19 Pneumonia: ARDS or not?, Critical Care 24, Article number 154 (2020)). In general, the role of specific pathogens for development of ARDS is considered to be difficult to assess (Acute Respiratory Distress Syndrome and Pneumonia: A Comprehensive Review of Clinical Data, Clinical Infectious Diseases, Vol. 43 Issue 6, 15 September 2006).
Pathological findings of an early COVID case study: overactivation of T cells
In one case concerning pathological findings of COVID-19 associated with ARDS, oxygen saturation remained above 95% until the fourteenth day of illness. Day 14 of the illness, hypoxaemia worsened and oxygen saturation dropped below 60%, followed by cardiac arrest. Bilateral diffuse alveolar damage with cellular fibromyxoid exudates was observed, as well as peeling of pneumocytes and hyaline membrane formation in the right lung; the left lung displayed pulmonary oedema with hyaline formation. These findings were regarded suggestive of early-onset ARDS. Mononuclear inflammatory infiltrates dominated by lymphocytes were seen in both lungs. One of major contributions to deterioration in this case was likely an overactivation of T cells. While peripheral CD4 and CD8 T cells were reduced, they were hyperactivated. High proportions of HLA-DR (presenting antigen and providing a ligand to T cells) and CD38 (glycoprotein on the surface of immune cells) were seen. Concentrations of CCR6+ Th17 (T-helper cells) were high, CD8 T cells were found to harbor high concentrations of cytotoxic granulates (Pathological findings of COVID-19 associated with ARDS, The Lancet, February 18 2020). Similar observations were made in a 2005 study (ACE2 Receptor Expression and SARS Infection Depend on Differentiation of Human Airway Epithelia, Journal of Virology, December 2005).
Cytokine storm and invasion of the Central Nervous System
Cytokine storm, an overreaction of the hosts' immune system, is coined to explain the mechanisms behind sudden deterioration (The cytokine release syndrome of severe COVID-19 and IL-6R antagonist Tocilizumab may be the key, International Journal of Antimicrobial Agents, 29 March 2020; see also Cytokine release syndrome in severe COVID-19, AAAS, 17 April 2020). Another pathway could be the invasion of the Central Nervous System and involving of the brain stem, which could explain patients' oxygen starvation. Both pathways have recently been rejected by researchers, as supplied data is still insufficient to prove that either cytokine storm or CNS involvement plays a major role in oxygen starvation- beside multiple organ failure.
Multi-factor assessment
Foremost, it must be noted that a homogeneous kind of ARDS does not exist. ARDS is a definition to describe acute onset of hypoxaemia (ARDS subphenotypes: Understanding a heterogeneous syndrome, Critical Care, 24 March 2020). Likewise, immunity response in SARS-CoV-2 patients is heterogeneous: treatment of immunity response is not a 'one size fits all' matter. This is even further complicated by the fact that immunomodulation should not impair antiviral activity in the host.
What should and could be learned from SARS-1 (2003) when it comes to assessing medical factors?
A comprehensive, multi-factor assessment could be of use to explain SARS' pathways from invasion to deterioration. The body is a system in which the affected parts each contribute to severity of disease. Immunity and cardiovascular mechanisms are intertwined, therefore these mechanisms cannot be considered to contribute independently to deterioration. These systems are a basic necessity to keep the machine going. I'd say that SARS causes imbalance in homestasis, characterized by ACE2 impairment and imbalance of the RAS, damage to endothelial tissue, instigation of the inflammatory soup/cascade, thrombotic events- given that these mechanisms enhance each other into an overdrive mode. The interplay between inflammation and venous thromboembolism is not simply one of cause and consequence, but an intertwined interaction. For example, see: 'The role of inflammation in Venous Thromboembolism', Frontiers in Pediatrics, 23 May 2018, 2018:6:142. What SARS-CoV-1 has made clear, is that coagulation disorders occur frequently in severe cases. Endothelial damage may be an early stage cause of an inflammation cascade, followed by thrombotic events. In a 2004 SARS review, it was said that the 2003 SARS epidemic experience should warrant increased vigilance against stroke and other thrombotic SARS-related events in future outbreaks of coronaviruses (Large artery ischaemic stroke in SARS, Journal of Neurology 251, October 2004).
I'll get to what has been intriguing me in the context of other disease case studies (cardiovascular) and what caught my attention again during the early phase of the SARS-CoV-2 pandemic: that is the plausible role of ACE2 as part of the RAAS system and the detrimental loss of ACE2 during infection with SARS-CoV-2.
The RAAS system and ACE
The Renin-Angiotensin-Aldosterone System (RAAS) regulates blood pressure and fluid balance. The RAS generates angiotensin II (Ang II), which binds to receptors in the brain, kidneys, vasculature and immune system. Angiotensinogen (Agt) is a substrate of renin. Renin cleaves Agt to Angiotensin I (Ang I), subsequently to be cleaved by ACE to Ang II. Renin is primarily expressed in the kidneys. Mast cells are involved in the release of renin. It was found in 2006 that release of renin by cardiac mast cells can be induced by ischemia (Classical Renin-Angiotensin System in Kidney Physiology, Comprehensive Physiology, Vol. 4 Issue 3, July 2014).
Bradykinin is a substrate for ACE. Bradykinin has vasodilator and natriuretic properties. ACE inactivates bradykinin and is therefore known as kininase II. ACE inhibitors increase the level of bradykinin (Unraveling the pivotal role of Bradykinin in ACE inhibitor activity, American Journal of Cardiovascular Drugs, 3 June 2016). The inhibition of ACE is associated with angioedema (Effect of bradykinin receptor antagonism on ACE inhibitor-associated angioedema, Journal of Allergy and Clinical Immunology, July 2017, Vol. 140 Issue 1).
ACE-AngII should be in balance with ACE2-Ang 1-7
ACE2 cleaves a residue from Ang I to form Ang 1-9 and converts Ang II to vasodilator Ang 1-7 (NCBI: gene ID), which blocks Ang II and inhibits ACE (ACE2, a new regulator of the renin-angiotensin system, Trends in Endocrinology and Metabolism, May 2004). In a 2008 study, it was proposed that loss of ACE2 expression and locally increased Ang II production triggered leakage of pulmonary blood vessels after SARS infection. Penninger mentions the catalytic inactivation of bradykinin metabolites by ACE2 (The discovery of angiotensin-converting enzyme 2 and its role in acute lung injury in mice, Experimental Physiology, 25 April 2008). Impairment of ACE2 during infection with SARS is likely the cause of disproportionate levels of bradykinin, which could lead to leakage.
Ang II is known to play a central role in endothelial dysfunction. Not only does Ang II increase blood pressure via vasoconstriction (the narrowing of blood vessels), actions on the Ang II type I receptor (AT1) adversely affects the vascular wall and enhances oxidative stress, resulting in endothelial damage and endothelial cell apoptosis. Oxidative stress increases expression of plasminogen activator inhibitor type I, resulting in the recruitment and binding of inflammatory cells to the endothelium, which leads to inflammation and thrombosis (A review of the role of bradykinin and nitric oxide in the cardioprotective action of Angiotensin-Converting Enzyme Inhibitors: Focus on Perindopril, Cardiology and Therapy 8, 1 October 2019).
Enhancement of ACE2 could be key (New agents modulating the renin-angiotensin-aldosterone system- Will there be a new therapeutic option?, Experimental Biology and Medicine, 19 July 2016). A recent follow-up of the 2008 study by Penninger proposes human recombinant ACE2 for another mechanism that seems plausible: the 2020 study shows inhibition of the virus by hrsACE2 (Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade hrsACE2, Cell Journal Pre-Proof, April 2020). Previously, a similar therapy was proposed involving recombinant human ACE2, rhACE2, to decrease plasma Ang II levels and increase Ang 1-7 and 1-5 (Recombinant human ACE2: acing out Ang II in ARDS therapy, Critical Care, 13 December 2017).
Next feature
In next feature, I will discuss the prevalence of thrombotic events and pulmonary embolism associated with SARS-CoV-1 (2003) and SARS-CoV-2. Twenty years of SARS has made clear that coagulation disorders occur in SARS cases- even patients who are casually deemed "not to be at risk" are in fact at risk of thrombotic events. Keep in mind that all of these mechanisms, from ACE2 impairment and dysregulation of the RAS, inflammation, thrombosis and thrombocytopenia (coagulation disorders) and cytokine storm are intertwined; these mechanisms and pathologies contribute to deterioration in severe cases of COVID-19.
Uncertainty: is ARDS an adequate classification?
It is yet unclear what exactly constitutes sudden deterioration in critically ill SARS-CoV-2 patients. A sudden deterioration in patients with oxygen deprivation is labelled "Acute Respiratory Distress Syndrome" (ARDS). It is prone to doubt whether ARDS, characterized by bilateral infiltrates, hypoxaemia and dyspnea (Acute Lung Injury and ARDS: Pathophysiology and Treatment, Missouri Medicine, Jul-Aug 2010), is an adequate classification for the pathophysiology associated with SARS-CoV-2 (COVID-19 Pneumonia: ARDS or not?, Critical Care 24, Article number 154 (2020)). In general, the role of specific pathogens for development of ARDS is considered to be difficult to assess (Acute Respiratory Distress Syndrome and Pneumonia: A Comprehensive Review of Clinical Data, Clinical Infectious Diseases, Vol. 43 Issue 6, 15 September 2006).
Pathological findings of an early COVID case study: overactivation of T cells
In one case concerning pathological findings of COVID-19 associated with ARDS, oxygen saturation remained above 95% until the fourteenth day of illness. Day 14 of the illness, hypoxaemia worsened and oxygen saturation dropped below 60%, followed by cardiac arrest. Bilateral diffuse alveolar damage with cellular fibromyxoid exudates was observed, as well as peeling of pneumocytes and hyaline membrane formation in the right lung; the left lung displayed pulmonary oedema with hyaline formation. These findings were regarded suggestive of early-onset ARDS. Mononuclear inflammatory infiltrates dominated by lymphocytes were seen in both lungs. One of major contributions to deterioration in this case was likely an overactivation of T cells. While peripheral CD4 and CD8 T cells were reduced, they were hyperactivated. High proportions of HLA-DR (presenting antigen and providing a ligand to T cells) and CD38 (glycoprotein on the surface of immune cells) were seen. Concentrations of CCR6+ Th17 (T-helper cells) were high, CD8 T cells were found to harbor high concentrations of cytotoxic granulates (Pathological findings of COVID-19 associated with ARDS, The Lancet, February 18 2020). Similar observations were made in a 2005 study (ACE2 Receptor Expression and SARS Infection Depend on Differentiation of Human Airway Epithelia, Journal of Virology, December 2005).
Cytokine storm and invasion of the Central Nervous System
Cytokine storm, an overreaction of the hosts' immune system, is coined to explain the mechanisms behind sudden deterioration (The cytokine release syndrome of severe COVID-19 and IL-6R antagonist Tocilizumab may be the key, International Journal of Antimicrobial Agents, 29 March 2020; see also Cytokine release syndrome in severe COVID-19, AAAS, 17 April 2020). Another pathway could be the invasion of the Central Nervous System and involving of the brain stem, which could explain patients' oxygen starvation. Both pathways have recently been rejected by researchers, as supplied data is still insufficient to prove that either cytokine storm or CNS involvement plays a major role in oxygen starvation- beside multiple organ failure.
Multi-factor assessment
Foremost, it must be noted that a homogeneous kind of ARDS does not exist. ARDS is a definition to describe acute onset of hypoxaemia (ARDS subphenotypes: Understanding a heterogeneous syndrome, Critical Care, 24 March 2020). Likewise, immunity response in SARS-CoV-2 patients is heterogeneous: treatment of immunity response is not a 'one size fits all' matter. This is even further complicated by the fact that immunomodulation should not impair antiviral activity in the host.
What should and could be learned from SARS-1 (2003) when it comes to assessing medical factors?
A comprehensive, multi-factor assessment could be of use to explain SARS' pathways from invasion to deterioration. The body is a system in which the affected parts each contribute to severity of disease. Immunity and cardiovascular mechanisms are intertwined, therefore these mechanisms cannot be considered to contribute independently to deterioration. These systems are a basic necessity to keep the machine going. I'd say that SARS causes imbalance in homestasis, characterized by ACE2 impairment and imbalance of the RAS, damage to endothelial tissue, instigation of the inflammatory soup/cascade, thrombotic events- given that these mechanisms enhance each other into an overdrive mode. The interplay between inflammation and venous thromboembolism is not simply one of cause and consequence, but an intertwined interaction. For example, see: 'The role of inflammation in Venous Thromboembolism', Frontiers in Pediatrics, 23 May 2018, 2018:6:142. What SARS-CoV-1 has made clear, is that coagulation disorders occur frequently in severe cases. Endothelial damage may be an early stage cause of an inflammation cascade, followed by thrombotic events. In a 2004 SARS review, it was said that the 2003 SARS epidemic experience should warrant increased vigilance against stroke and other thrombotic SARS-related events in future outbreaks of coronaviruses (Large artery ischaemic stroke in SARS, Journal of Neurology 251, October 2004).
I'll get to what has been intriguing me in the context of other disease case studies (cardiovascular) and what caught my attention again during the early phase of the SARS-CoV-2 pandemic: that is the plausible role of ACE2 as part of the RAAS system and the detrimental loss of ACE2 during infection with SARS-CoV-2.
The RAAS system and ACE
The Renin-Angiotensin-Aldosterone System (RAAS) regulates blood pressure and fluid balance. The RAS generates angiotensin II (Ang II), which binds to receptors in the brain, kidneys, vasculature and immune system. Angiotensinogen (Agt) is a substrate of renin. Renin cleaves Agt to Angiotensin I (Ang I), subsequently to be cleaved by ACE to Ang II. Renin is primarily expressed in the kidneys. Mast cells are involved in the release of renin. It was found in 2006 that release of renin by cardiac mast cells can be induced by ischemia (Classical Renin-Angiotensin System in Kidney Physiology, Comprehensive Physiology, Vol. 4 Issue 3, July 2014).
Bradykinin is a substrate for ACE. Bradykinin has vasodilator and natriuretic properties. ACE inactivates bradykinin and is therefore known as kininase II. ACE inhibitors increase the level of bradykinin (Unraveling the pivotal role of Bradykinin in ACE inhibitor activity, American Journal of Cardiovascular Drugs, 3 June 2016). The inhibition of ACE is associated with angioedema (Effect of bradykinin receptor antagonism on ACE inhibitor-associated angioedema, Journal of Allergy and Clinical Immunology, July 2017, Vol. 140 Issue 1).
ACE-AngII should be in balance with ACE2-Ang 1-7
ACE2 cleaves a residue from Ang I to form Ang 1-9 and converts Ang II to vasodilator Ang 1-7 (NCBI: gene ID), which blocks Ang II and inhibits ACE (ACE2, a new regulator of the renin-angiotensin system, Trends in Endocrinology and Metabolism, May 2004). In a 2008 study, it was proposed that loss of ACE2 expression and locally increased Ang II production triggered leakage of pulmonary blood vessels after SARS infection. Penninger mentions the catalytic inactivation of bradykinin metabolites by ACE2 (The discovery of angiotensin-converting enzyme 2 and its role in acute lung injury in mice, Experimental Physiology, 25 April 2008). Impairment of ACE2 during infection with SARS is likely the cause of disproportionate levels of bradykinin, which could lead to leakage.
Ang II is known to play a central role in endothelial dysfunction. Not only does Ang II increase blood pressure via vasoconstriction (the narrowing of blood vessels), actions on the Ang II type I receptor (AT1) adversely affects the vascular wall and enhances oxidative stress, resulting in endothelial damage and endothelial cell apoptosis. Oxidative stress increases expression of plasminogen activator inhibitor type I, resulting in the recruitment and binding of inflammatory cells to the endothelium, which leads to inflammation and thrombosis (A review of the role of bradykinin and nitric oxide in the cardioprotective action of Angiotensin-Converting Enzyme Inhibitors: Focus on Perindopril, Cardiology and Therapy 8, 1 October 2019).
Enhancement of ACE2 could be key (New agents modulating the renin-angiotensin-aldosterone system- Will there be a new therapeutic option?, Experimental Biology and Medicine, 19 July 2016). A recent follow-up of the 2008 study by Penninger proposes human recombinant ACE2 for another mechanism that seems plausible: the 2020 study shows inhibition of the virus by hrsACE2 (Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade hrsACE2, Cell Journal Pre-Proof, April 2020). Previously, a similar therapy was proposed involving recombinant human ACE2, rhACE2, to decrease plasma Ang II levels and increase Ang 1-7 and 1-5 (Recombinant human ACE2: acing out Ang II in ARDS therapy, Critical Care, 13 December 2017).
Next feature
In next feature, I will discuss the prevalence of thrombotic events and pulmonary embolism associated with SARS-CoV-1 (2003) and SARS-CoV-2. Twenty years of SARS has made clear that coagulation disorders occur in SARS cases- even patients who are casually deemed "not to be at risk" are in fact at risk of thrombotic events. Keep in mind that all of these mechanisms, from ACE2 impairment and dysregulation of the RAS, inflammation, thrombosis and thrombocytopenia (coagulation disorders) and cytokine storm are intertwined; these mechanisms and pathologies contribute to deterioration in severe cases of COVID-19.
 |
| The RAS and its relation to inflammation and coagulation disorders in COVID-19 |
In summary: slides